What is Obesity?
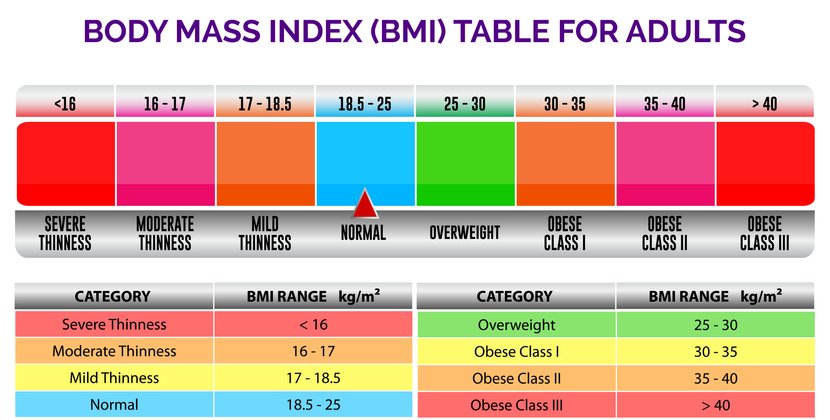
The World Health Organization (WHO) defines obesity as “abnormal or excessive fat accumulation that presents a risk to health”. The most common way we measure obesity is by using a calculation known as BMI (body mass index).
A body mass index (BMI) greater than 30 is considered obese. It’s important to note that BMI is not a perfect tool. It does not consider age or sex and does not differentiate between muscle and fat tissue. Therefore, a fit person with a lot of muscle mass may have a high BMI. As such BMI in isolation may not be a reliable indicator of eligibility for bariatric surgery.
Using BMI as a tool in 2016, it was thought that more than 1.9 billion adults globally were overweight and over 650 million adults were obese.
There are many many factors which contribute to obesity including modern living, family history, genetics and an energy imbalance (consuming more calories than are used).
Health Risks of Obesity
Elevated BMI is considered a major contributing factor for the following conditions:
Heart disease including high blood pressure and stroke
Respiratory disease including obstructive sleep apnoea
Diabetes
Disorders of the musculoskeletal systems including osteoarthritis
Some cancers including endometrial, breast, ovarian, prostate, kidney and colon
Infertility and pregnancy complications
The higher the BMI, the greater the risk of the above disorders. Obesity can also impact negatively on mental health, self esteem and an overall ability to participate in and enjoy life.
Permanent changes to diet and lifestyle such as limiting energy intake from total fats and sugars and engaging in regular exercise is the first line treatment for obesity. Prescription appetite suppressant medication may also be considered. The higher the BMI the more difficult it can be to maintain any weight loss achieved long term with diet and exercise alone.
Surgery as a Tool to Assist with Weight Loss
Where lifestyle changes have been unable to achieve or maintain weight loss and a person's health is at risk, surgical options may be considered. We encourage careful consideration and discussion with your General Practitioner, any specialist health care provider you might have as well as with a trusted support person and potential surgeon before deciding if surgery is right for you.
You may be a candidate for weight loss surgery if:
You have been unsuccessful maintaining or achieving weight loss in the past
Your excess weight is limiting and affecting your ability to live a fulfilling, active and happy life, including your ability to socialise and exercise
Excess weight is impacting your health and other medical issues. In this situation patients often state their general practitioner or physician wants them to lose weight.
You are prepared to change your eating and lifestyle behaviours
You are older than 18 years of age
Your BMI is greater than 30kg/m2
If your General Practitioner has referred you for weight loss surgery, please advise them to order the following blood tests.
Surgical Options
Weight loss surgery is one of the most effective tools available to assist you with losing weight and improving your health and wellbeing.
Our surgeons and allied health team provides support that will allow you to best utilise this tool to achieve your long-term weight loss goals and weight maintenance thereafter. We believe that continuity of care is critical to weight loss success and as such, it is important to seek support from your general practitioner, dietitian, psychologist and quit smoking.
Your surgeon will be able to address any questions or doubts you may have about weight loss surgery, explain the details of each type of surgery and discuss which option will best suit your individual health needs and weight loss goals.
What happens after you have been approved for weight loss surgery?
Before you proceed to surgery, you will be asked to have a blood test.
Before booking in for weight loss surgery, you will need to have a gastroscopy. A gastroscopy is a day procedure where you are given a light anaesthetic (sedation), and a surgeon uses a camera, or endoscope, to assess your oesophagus and stomach. This procedure only takes about 10 minutes and is a safe way to assess for any symptoms of things such as reflux or oesophagitis, which will help to determine the most appropriate type of weight loss surgery for you.
At your next appointment, your surgeon will discuss the results of your gastroscopy with you and advise on what weight loss procedures are suitable for you. Once the decision is made with yourself and your surgeon, they will talk you through all the risks involved, and sign surgical consent paperwork with you once you have had time to ask any questions that you may have.
Pre-Operative Diet
When you have a date for surgery, you will be advised to follow a very low-calorie liquid meal replacement diet (VLCD) for 14 days prior to surgery. OptifastTM is the recommended meal replacement and is available from your local Chemist. This diet helps you to lose weight, particularly from the liver, and therefore optimises the safety of the procedure. You will receive more detailed information about this when you see your dietitian.
Post-Operative Care
The hospital stay after surgery is generally three to five days. After the procedure you will start on clear fluids only (water, black tea, broth, juices). These will need to be sipped slowly in small amounts. An x-ray study is performed after the operation to check the size of the stomach pouch and to exclude a leak from the stapled edge of the stomach. You will then be able to have free fluids for the rest of your hospital stay. During the next 4 to 6 weeks, while your body heals, you will gradually increase the texture and volume of the food you take. Further information, including a dietary guidelines booklet, will be provided at your appointment with the dietitian.
Appointments
The first post-operative clinic visit will be arranged about 1 to 3 weeks after surgery. At this appointment your wounds will be assessed, and any other issues will be discussed.
Please note:
Every surgery can have risks and complications which you should already be aware of from your consultation and consent with the surgeon. Your appointments or bookings could change or be cancelled due to patients with emergency or priority needs. You may not be booked for surgery without meeting your doctor’s recommendations.

Contact Details
Elective Surgery Surgical Liaison Nurse:
(03) 9231 2401
Elective Surgery Waiting List Officer:
(03) 9231 2976
Fax: 9231 3224
Dietitian:
(03) 9231 3756